Current Work - My Prostate Cancer Journey - Chapter 2
This follows on from Chapter 1, my Radiotherapy Sketchbook, which covers my prostate cancer journey up until the 2nd December 2021.
20 December 2022
I always thought my prostate cancer would come back sooner or later
It now looks as though itís sooner.
My PSA, the amount of ďprostate specific antigenĒ in my blood, was 0.05 on the 27th July 2022 but had risen to 0.21 three months later. Although thatís still very low itís a cause for concern because Iím still on hormone therapy, which is meant to starve my cancer of testosterone and prevent it growing.
Apparently prostate cancer can become hormone-resistant.
As a result of this I had a PET scan on the 9th December to get a detailed view of whatís going on inside my body. Iím getting the results and, hopefully, a treatment plan tomorrow, when I see my consultant at Derriford Hospital.
As usual, I feel as fit as a fiddle.
21 December 2022
Good news on my prostate cancer. The results of the PET scan I had on the 9th December indicate that it hasnít spread - itís not in my bones, itís not in my lymph nodes.
Phew!
Where it appears to be growing is back inside my prostate gland. Apparently itís a little tricky dealing with it there, partly because itís already undergone 2 rounds of radiotherapy and partly because the gland is close to where my colon/rectum were sewn back together after Iíd had a section removed during my bowel cancer operation in 2011.
The current plan for this is to put e on an additional drug, Darolutamide, once my PSA gets to 2. The medics are also seeing whether Iím ďsuitableĒ for a pioneering ultrasound treatment being conducted in Southampton.
I can live with thatÖÖliterally!
28 March 2023
Iíve had a chat with the consultant in charge of my treatment for prostate cancer today.
Good news: My PSA, the level of prostate specific antigen in my blood, was 0.24 on 16th March, no change from what it was on 27th January. Thatís very low - under normal circumstances medics donít take much interest until PSA levels gets to 4 or above.
However, Iím an oddity so we had a discussion about my treatment going forward, bearing in mind my current state:
The cancer seems to back inside my prostate gland. The radiotherapy I had in November 2021 appears to have killed off the stuff that was in a couple of lymph nodes outside the gland, butÖ
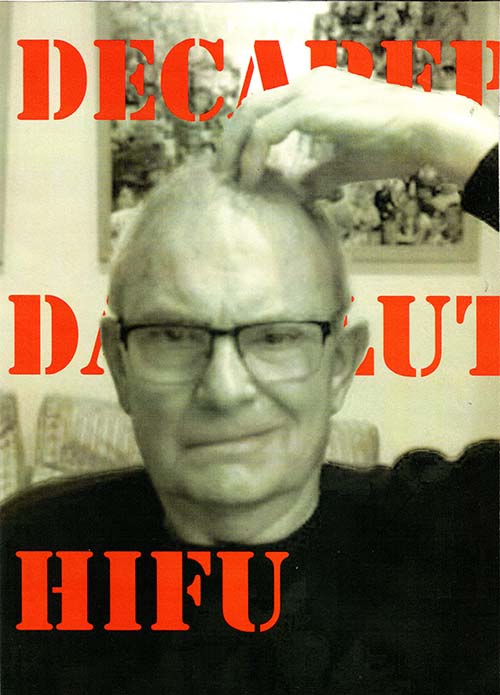
The cancer might be becoming resistant to the hormone treatment Iím on, an injection of Decapeptyl in the bum every 3 months.
One option is to wait and until my cancer has grown and then start taking another drug, Darolutamide. Initially I was told the trigger point was a PSA of 2 but it now seems to be when my PSA is doubling in 10 months or less. Both seem a long way off at present. My consultant says Iíve got ďseveral yearsĒ at least.
The other option is to have High-intensity focused ultrasound (HIFU) treatment which MIGHT destroy the tumour - ie rid me completely of prostate cancer and allow me to stop having hormone therapy.
Note the ďMIGHTĒ. Theyíve never tried HIFU on someone with my background so they have no data on which to predict the outcome, my consultant says. The background - scar tissue surrounding my prostate gland from my bowel cancer op in 2011 and other damage from my previous rounds of radiotherapy in 2013 and 2021 (which precludes me having any more radiotherapy, apparently).
To make matters more interesting, HIFU needs to be done when the tumour is small - ie, soon(ish). It wonít work if I wait for my PSA to increase. And like most medical therapies there are risks, similar in type and scale to those for radiotherapy, which so far Iíve avoided.
So itís a gamble
Iím going to go for it. At least, Iíve asked my consultant to contact the outfits offering HIFU to see whether one of them will take me on.
9 June 2023
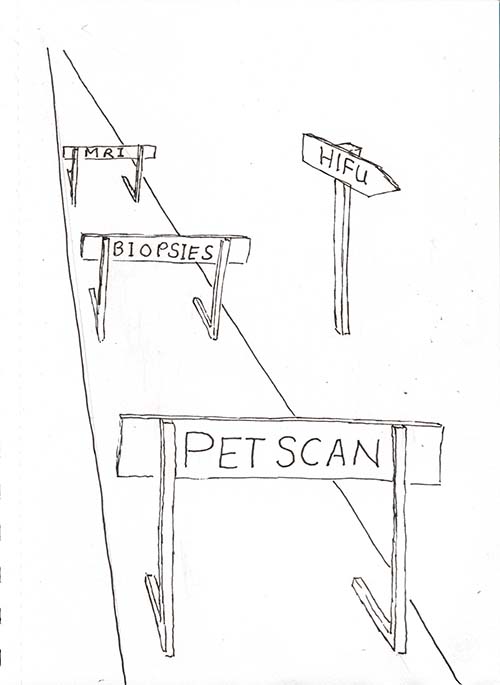
HIFU treatment is only suitable for early stage prostate cancer - where the tumours are small and within the prostate gland - the cancer hasnít spread elsewhere.
Hence me facing a succession of hurdles to prove this is the case - an MRI scan which I had on the 22nd May, biopsies today, and yet another PET scan some time in the future.
I got the results of the MRI scan today. They confirm the previous PET scan results - the radiotherapy I had in 2021 killed off the cancer in the lymph nodes outside the prostate gland. I knew something was going on INSIDE the prostate gland and the MRI scan indicates 2 small areas that might be tumours. One of them is rated 4 out of 5 in terms of its likelihood of it being a tumour and the other is 3 out of 5.
Hence todayís biopsies - taking samples of these potential tumours which are now being sent away for analysis.
I was expecting the procedure today to be quite unpleasant but it wasnít as bad as I feared. It started off with me stripping off, putting on a gown and having to wear a jock-strap. I was then put in a special chair so they could raise my legs up and expose my perineum - the area between my legs. A sonic probe was stuck up my arse so my insides were visible on a screen, which enabled them to steer a sort of flexible hollow needle into my prostate gland and take tiny samples of the suspected tumours.
I was expecting this to hurt but it was just mildly uncomfortable. And watching what was happening on the screen was really interesting. At one stage they pointed to some white spots and told me it was damaged tissue resulting from the high-dose-rate brachytherapy in 2013. I was really surprised that it was still visible 10 years after Iíd had the procedure.

10 June 2023
Yesterdayís prostate biopsy resulted in a scary time last night. I was told to expect blood in my pee for a couple of days afterwards and to drink lots of water to flush it away. I did but I guess it wasnít enough. I got a blockage. I was busting for a pee but when I tried all I got was a dribble of blood and an occasional black clot.
I kept on trying and got steadily more alarmed. I thought about driving to A&E but wasnít sure whether I could last another hour. By midnight I was desperate and called 111. The triage process resulted in me being told that a doctor would phone me.
I waited and waited and waited, getting more and more worried. I kept on trying to pee and getting the same result - a dribble of blood. At 2am I tried extra hard and the dam burst - blood, black clots and pee everywhere. I cleaned up and went to bed but had to keep on getting up for a repeat performance.
By the morning the worst was over. I was able to pee on demand and it was almost colourless. A doctor finally phoned at 8:30. She said she had tried phoning at 2:30. She also said that the 111 triage process should have marked my case as top priority/urgent when I said I had a urinary blockage, and that someone would have come to my house with a catheter to sort me out.
Iíll know for next time, but I hope there isnít one - it was a scary experience.
5 July 2023
Update on my prostate cancer journey: My oncology consultant phoned on Monday to give me the results of the biopsies. All as expected - 2 small tumours inside the prostate gland.
We had another discussion on the relative merits of HIFU ultra-sound treatment to kill off the tumours (which might have side effects similar to radiotherapy) or continuing with hormone treatment and eventually switching to another drug to keep things under control (which could be several years into the future).
It's a balance of risks. My consultant thinks HIFU edges it, which is what I think also - I'd like to get off hormone therapy which makes me have hot flushes and sweats, and makes me flabby. And so far my body has stood up well to 2 rounds of radiotherapy - no side effects.
So we're moving to the next step. My consultant is referring me to a HIFU specialist, a consultant in Southampton whom he knows and who is super-cautious, will want to make sure himself that I'm a suitable candidate for HIFU before going ahead. Looks like I'll have to pay for it - can't get it on the NHS.
I'm having a PET scan tomorrow to double check that the cancer hasn't spread outside my prostate gland. My consultant thinks this is just belt and braces - just helping the guy in Southampton make a decision in my favour - because I had a PET scan only 6 months ago that indicated things hadn't spread.
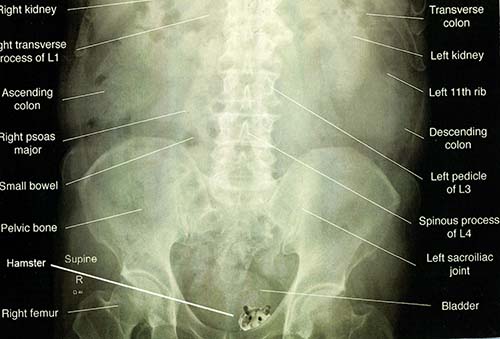
PET (for Positron Emission Tomography) scans produce very detailed 3D images of the inside of the body. They highlight abnormalities and indicate how well certain functions of the body are working. Youíre injected with a radioactive liquid before being put through a doughnut-type CT scanner. Scanning my abdomen takes 40 minutes. I have been known to fall sleep in these things although I know some people suffer claustrophobia in them.
The illustration is a visual pun of a PET Scan. Excuse my juvenile humour.
28 July 2023
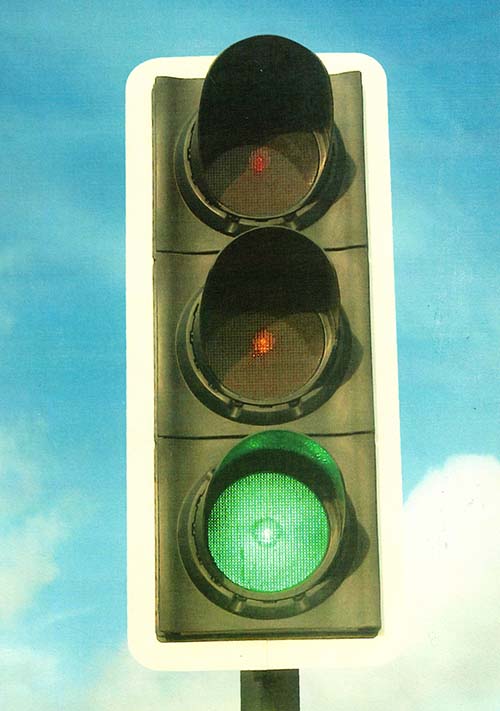
Breaking news: Iíve got the go-ahead for some specialised treatment of my prostate cancer - the result of proposals from a pioneer in this field, Tim Dudderidge, being discussed by a multi-discipline team of experts in Southampton today.
The specialised treatment might use HIFU ultra-sound to zap a couple of small tumours in my prostate gland. Alternatively they might use cryotherapy - freezing the tumours to kill them off.
Right now I donít know which of these treatments will be used and I donít know the timescale for the procedure. All Iíve got to go on this evening is a voice-mail from Dudderidge, telling me heís got the green light.
The big issue with HIFU and cryotherapy - the one discussed by Dudderidge and his colleagues in todayís meeting - is that my prostate is right next to my colon/rectum, a section of which was chopped out when I had an operation for bowel cancer in 2011. They want to make sure they donít hit the so-called anastomosis, where my guts were sewn back together.
Dudderidge went back to the surgeon that did my 2011 op to try and pin down the position of my anastomosis. And he says he has ways of pushing my guts away from my prostate gland anyhow. But of course there are risks, as there are with all medical procedures.
The idea (or hope) is that this will rid me of prostate cancer altogether and I can come off hormone therapy, which gives me hot flushes, sweats and flabbiness.
If I didnít have this HIFU or cryotherapy treatment I would have to stay on hormone therapy and there are signs that my prostate cancer is becoming resistant to it. In the long run (maybe several years) I would probably have to move on to a different drug, and all of these seem to have side-effects.
11 September 2023
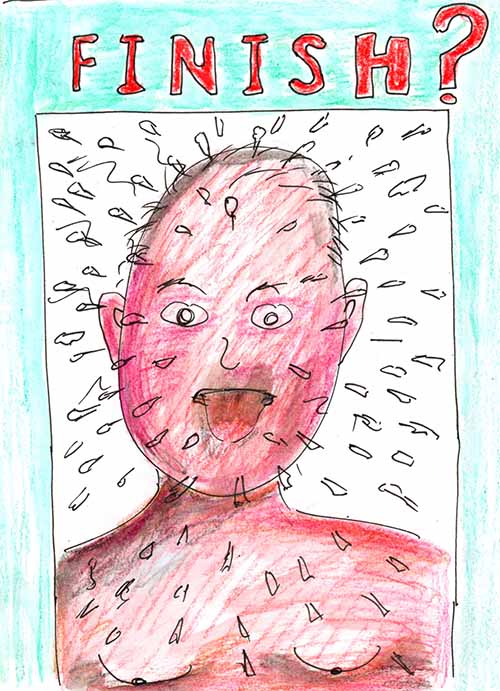
This picture is of me enduring what women have to go through at a certain age - the menopause - hot flushes, sweats and flabbiness. I always was prone to sweating but now I boil and sweat absolute buckets at the drop of a hat - any exercise or feeling just a teeny-weeny bit stressed. Getting stuck on a crossword clue is a big enough trigger and feeling self-conscious about my sweating aggravates everything.
At night no triggers are needed: I wake up every now and again, boiling hot and running in sweat. Notice, also, that Iíve grown small tits and lost the hair on my chest.
This is all caused by the hormone therapy, also known as ďchemical castrationĒ (yikes!) that I started in the Spring of 2021. I have a jab of Decapeptyl in my bum every 3 months that aims to stop me producing testosterone, which is what prostate cancer ďfeedsĒ on. Whatís left in my body is the female sex hormone, oestrogen - hence me having menopause symptoms.
As you may have seen from my previous posts, it looks as though my cancer is getting resistant to Decapeptyl. My PSA, the unreliable method of measuring prostate cancer, is increasing, although itís still really low - 0.31 on 4th September. Under the NHS I would continue with Decapeptyl until my PSA was doubling every 10 months when I would be eligible to move on to another (expensive) drug.
However Iíve opted for an alternative (private) treatment, cryotherapy, which Iím having in 10 days time in Southampton. More about this in a separate post. Iím hoping that this will get me off hormone treatment and eventually halt the side effects. This is likely to take some time. My last Decapeptyl injection was only a week ago and itíll take a long time to wash out of my system. In fact, someone I know stopped hormone therapy a long time ago and still gets hot flushes, so I need to manage my expectations!
13th September 2023
For the past year Iíve been participating in a clinical trial to see whether exercise alleviates the side effects of hormone therapy for prostate cancer. Iíve been going to a gym in Plymouth twice a week for sessions of cardio and resistance exercises.
I keep a record of my exercises, pictured, summaries of which are shared with the medical researchers running the trial.
Every 3 months the researchers weigh me, measure my waist and hips, take my blood pressure and assess my fitness by getting me to sit down on a chair and stand up again as many times as I can in 30 seconds. In an assessment last Monday I achieved 34 - one better than my previous test (when I broke the chair!).
Hundreds of men are participating in this nation-wide trial and 30 or 40 of them go to the same gym as me. Meeting them has been quite an eye-opener. Although weíre all on hormone therapy for prostate cancer weíre at different stages of the disease, have different histories and prognoses, and suffer different side effects.
Nobody sweats like me in the gym - I am drenched after an hour. On the other hand I donít suffer at all from fatigue, another common side effect. A lot of the men look knackered and donít put much effort into the exercises. In contrast I push myself and feel as fit as a flea. Maybe thatís why Iím willing to put up with the sweating?
FYI, hereís a list of common side-effects of hormone therapy:
* loss of interest in sex (lowered libido)
* erectile dysfunction
* hot flushes
* loss of bone density
* bone fractures
* loss of muscle mass and physical strength
* changes in blood lipids
* insulin resistance
* weight gain
* mood swings
* fatigue
* growth of breast tissue (gynecomastia)
17th September 2023
The medical procedure Iím going to undergo for my prostate cancer next Thursday (21st September) - cryotherapy - reminds me of toasting marshmallows in a fire.
In my case, the marshmallow is my prostate gland (normally the size of a walnut but apparently mineís quite small, which helps with cryotherapy). The stick is my urethra, the ďpipeĒ that passes through my prostate gland and carries urine away from my bladder through my penis.
Continuing the metaphor, the ďtrickĒ with cryotherapy is to burn away the marshmallow completely without even scorching the stick - although it's the opposite of burning, it's freezing. Itís a specialised treatment only available in a few places and Mr. Dudderidge, a surgeon in Southampton, is considered to be a pioneer in this field.
So, hereís how itís done:
Dudderidge will guide several hollow needles up between my legs into my prostate gland using an ultrasound probe up my arse so he can monitor what's happening on a computer screen. Heíll pass very cold gas through the needles to freeze and destroy the gland at the same time as passing warm salt water through a catheter in my urethra to prevent it getting damaged.
I think they also might do something to push my anastomosis (where my guts were sewn back together after my bowel cancer op), away from the prostate gland, possibly by giving me an enema and filling my bladder (as they did in my last round of radiotherapy).
All of this is done under a general anaesthetic (thank heavens!).
This procedure is only suitable for early stage cancer when it's still contained inside the prostate gland. I'm somewhat unusual in that the cancer HAD got outside my gland, into 2 lymph nodes, but the radiotherapy I had in 2021 appears to have rectified that. However a couple of tiny tumours have started growing inside my gland indicating that the cancer has become resistant to hormone therapy.
I've had various scans and tests to convince Dudderidge and his colleagues that cryotherapy is appropriate.
All the same, I've been told that the outcome canít be predicted with the usual levels of confidence because of what Iíve already been through - the bowel cancer op and two rounds of radiotherapy. But my oncology consultant, who I trust, trusts Dudderidge and says he wonít take unnecessary risks.
So, gulp, wish me luck!!
8 October 2023
Medical mayhem last night. I got home after visiting Beryl in hospital (she's had an operation on her stump) and had another urinary blockage, following my cryotherapy on 21st September. Hoped it would unblock itself, gave up and phoned 111 at 8pm, had to wait until 1:30am for a doctor to rescue me. In the interim I'd got desperate, phoned 999, was told to drive to A&E, knew that would take too long, tried sticking a plastic tube up my penis.
12 October 2023
An update on my medical situation.
The catheter that was installed early Sunday morning was very uncomfortable, verging on painful, almost torture. I've finally removed it and am much relieved. I waited until Spire had sent me a big pack of "intermittent catheters" (which they should have given me on discharge) so I can "rod" myself if I get another urinary blockage.
As it happens I had a phone appointment with my oncology consultant yesterday. He told me not to remove the catheter myself - "there's a process to follow" - and that he would arrange for this to be done in hospital as a matter of urgency.....which would be "about 4 weeks". "Four weeks!!!!!!!" I shouted, "I need it now, it's hurting me.Ē
I then told him Spire was sending me some intermittent catheters. Again he said I needed to be trained to use them.
Anyhow, I really like my oncology consultant and trust him but I've ignored his advice.
I had some bloods taken last Thursday while Beryl was having an operation on her stump. The results indicated that my PSA (the unreliable way of measuring prostate cancer) was 0.34, up from 0.31 a few weeks ago. I was hoping it would be zero after the cryotherapy, which supposedly killed off all the detectable cancer. But apparently it takes a while for this to register in the blood.